Learned the Hard Way
You would think that growing up with juvenile rheumatoid arthritis, I'd be well aware of my limits and abilities, and know when I was pushing myself too hard, too far or too fast. Or all three even. On one hand, not doing those things makes perfect sense. It's safe, you're unlikely to hurt yourself easily, or bring on a flare by overdoing things or going full speed ahead. Of course this does not mean you will be free of flares and pain. That's part of the nature of having an autoimmune arthritis disease---flares and pain, along with swelling, redness in the joints, vasculitis, lung problems, eye problems, heart problems, well, you name it and autoimmune arthritis is more than likely able to affect it in one way or another. Even for one whose disease is mild or one who has had a great response to medications flares are still part of the deal. It's just part of life with a chronic illness. Some people get used to it, others don't. Below I will discuss how flares, the weather, sleep, stress, pushing too hard, and self-care affect a person with RA, fibro or other chronic illnesses. Then I tell about how I didn't take care of myself as well as I should have and ended up in the hospital for 11 months and then spent another 2 years in a nursing home learning to take care of myself again before I was able to come home.
Flares
flare up (aka flare) noun a sudden outburst of or increase in the symptoms of a disease or condition.Flares can last hours, days, weeks, or months. Their severity can be mild, moderate, severe, or "kill me now". Ok, so while I'd not seriously want to be killed, a bad flare can make you facetiously wish to be put out of your misery!
 |
| The FLARE game from RA Guy |
A lot of people say they feel like they're dealing with the flu to the tenth power during a flare. There are a number of things that can bring on a flare: doing too much; bad weather; not practicing good self-care; stress (both bad stress and good stress such as the stress associated with happy events such as a vacation; having company visiting; weddings, etc.); an acute illness such as a cold or the flu; not sleeping enough; missing medications whether due to spacing out and forgetting them, skipping them to make them last longer or running out for whatever reason; pushing yourself too hard; no longer being responsive to medications, etc.
During a flare, everything that can hurt usually does. I am tired --- physically worn out, mentally tired, and sleepy all at the same time. How I can be sleepy after 12-18 hrs of sleep is beyond me, but it happens. Oh wait, for sleep to be good, one needs to be able to enter all of the stages of sleep, not just the early stages of sleep.
Weather
 |
| Hurricane Hanna 09/06/08 Hit SC/NC border 3am |
One thing I find odd, is my flare pattern during a tropical event such as a tropical storm or hurricane. I might have a small flare as the front approaches, usually nothing too bad; unless I'd already been flaring prior to the front approaching. Once the front hits and the barometric pressure drops to the rate typically seen with a tropical system, I feel almost energized. That's an odd feeling for me, since most tropical systems produce at least some rain and I normally do NOT react well to rain. Typically, rain causes me to feel each painful joint all the more than I normally do. I become very stiff, occasionally swollen (although swelling is rare for me), and I have a lack of energy that is worse than my normal lack of energy. My whole body is tender to the touch (it's as if even my hair hurts). I feel as if my limbs are encased in concrete, making them feel heavy and hard to move. During this time, my fibro fog worsens. But, during the tropical low pressures associated with hurricanes and tropical storms, I feel an energy I typically do not possess (but wish I had). The stiffness relents, the mental fog parts, I no longer feel as if moving takes serious weight lifting. It's almost as if I have my pre-fibro self back. It does not last very long at all though, but even a few hours of relief is nice.
Sleep
There are two main stages of sleep: non-rapid eye movement (NREM) and rapid eye movement (REM). NREM is also known as quiet sleep; REM is known as active sleep. In the beginning of sleep you are fairly awake and alert. Strange and vivid sensations, known as "hypnogogic hallucinations" occur. These sensations, such as feeling as if you are falling, or hearing someone call your name, can happen during this stage. Theta waves, very slow brain waves, occur during this time.
 |
| Wayney asleep on the keyboard tray. |
Stage 2 sleep lasts approximately 20 min.. During this stage, body temperature decreases, the heart rate begins to slow and sleep spindles, which are bursts of rapid, rhythmic brain wave activity, are starting to be produced by the brain.
In stage 3 sleep, delta waves, which are deep, slow brain waves, begin to emerge during this transition between light sleep and very deep sleep.
Stage 4 sleep is referred to as delta sleep, because the delta waves that start in stage 3 continue, triggering a deep sleep which lasts approximately 30 minutes.
Stage 5 is when REM sleep happens. During this stage, there is eye movement, increased respiration, increased brain activity and dreaming. This stage is also referred to as paradoxical sleep because even though there is more activity in the brain, the muscles relax more.
Sleep does not progress through the stages in sequence. Stages 1-4 progress normally, then stage 3 is repeated. After this, second cycle of stage 3 sleep, the body enters stage 2 again and then enters the REM stage approximately 90 min. after falling asleep. This cycle occurs 4-5 times per night, with the first cycle of REM being a short lasting stage. Each cycle, the REM stage sleep becomes lengthened to as long as an hour per cycle.
I have learned that sleep is important when dealing with chronic illness. Good sleep will help you in managing your other symptoms. Unfortunately, sleep is very hard for us to get, Pain, muscle spasms, being a light sleeper, waking to go to the restroom etc. all cause sleep interruptions. Once sleep is interrupted, it is very hard to get back to sleep. Sometimes, when you get sleep enough, you'll sleep anywhere or if you've had a trouble sleeping, you'll find yourself just dosing off while doing other things.
Stress
Stress can either be caused by flare, or can be the cause of flares. As noted earlier, even what we consider to be "good stress" can affect how we feel in a negative way. Anytime we feel stress, good or bad, our body is likely to respond. It cannot tell the difference between good or bad stress, so it reacts accordingly. Flares can be emotional times for us, and stress on top of a flare just adds to the emotional load. We need to learn to manage stress and not let it manage us. Chronic illness plus stress will just lead to additional pain; that increased pain increases our stress, making our chronic illness flare even worse. It becomes one vicious, huge cycle of stress, pain and chronic illness.
There are various ways of managing stress. One thing about learning to manage stress is that every person is different in what they find stressful. For one person, the thing that relieves their stress is a major trigger in a different person. We must remember not to judge others for their choices in what relieves stress so long as they are not causing further problems for themselves or someone else. Some people cannot comprehend gardening as being a stress reducer and others find it a huge reliever of stress. That shows how each person must look for their own way to manage stress, and keep trying new things until you find what works for you.
Pushing too hard or too fast
 Some people just plain push themselves WAY too hard. I've done it myself many times. And in the end, I more than likely paid dearly for doing so. How? Because by overdoing it, I did not allow my body a chance to slow down, to use its built in repair mechanism to repair itself as much as it could, relax and get rest, not sleep, but rest, as in being still, not moving all the time, not getting up and doing this or that just to stay busy. In doing so, all of the factors that influence a flare were able to join forces and wage an all out flare war on my body.
Some people just plain push themselves WAY too hard. I've done it myself many times. And in the end, I more than likely paid dearly for doing so. How? Because by overdoing it, I did not allow my body a chance to slow down, to use its built in repair mechanism to repair itself as much as it could, relax and get rest, not sleep, but rest, as in being still, not moving all the time, not getting up and doing this or that just to stay busy. In doing so, all of the factors that influence a flare were able to join forces and wage an all out flare war on my body.
One thing that those of us who have a tendency to push too hard need to remember is that we are human BEINGS not human DOINGS! By that, I mean that sometimes we get so caught up in our activities that our view of self revolves around what we do, not who we are; we see ourselves as our career. How many of you identify yourself through your job? Even if you no longer work, do you find yourself saying, "I am a teacher." or "I work in the aerospace engineering field.", even if you know that you will not being able to return to that job or any other job for that matter. I used to do that, but after awhile, it got old explaining why. So, I began to refer to myself not in terms of what I used to do as a job, but in terms of who I AM --- a wife and mother. I began to see not working as a blessing in a way. It allowed me to spend more time with my son. I also got to "work" more with the support groups with which I was involved. By "work", I mean just reading and answering posts, answering questions that group members had, and putting out a newsletter on the relevant subjects to the group's focus. In order to do these jobs, I needed to read through approximately 1000+ newsletters per week as well as keeping up with the group posts, some of which required a bit of research. I kept fairly busy, which ended up leading to getting burnt out. I learned the hard way that I must not get so busy that I became a human doing rather than a human being.
pace oneself verb do something at a restrained and steady rate or speed.
In other words, to not do something too quickly so that one does not get too tired or to finish.
I must learn to pace myself. How do I do that? I break tasks into small manageable steps. I set a limit of working for a time, then taking a break. Different tasks will mean that the time you can work on them, then take a a short break and then go back to the job will be different. Some parts of a job may need to be done all at once. If so, do the job and then adjust your rest period accordingly.
pace oneself verb do something at a restrained and steady rate or speed.
In other words, to not do something too quickly so that one does not get too tired or to finish.
I must learn to pace myself. How do I do that? I break tasks into small manageable steps. I set a limit of working for a time, then taking a break. Different tasks will mean that the time you can work on them, then take a a short break and then go back to the job will be different. Some parts of a job may need to be done all at once. If so, do the job and then adjust your rest period accordingly.
Self-Care
 Another factor in flares is not taking good care of yourself, or taking care of everyone around you at the expense of not giving yourself enough care. As women, we are taught to be the caretakers. But, one thing we, especially those of use with chronic illnesses, absolutely MUST remember is that we cannot take care of those around us if we do not meet our own needs properly as well. Sometimes, even though it may feel somewhat selfish (and against all that we are taught is part of being a great wife, mother, employee, friend, etc.), we MUST make time to care for ourselves. At times, we need to do this before we can meet the needs of those around us. It is hard to do this as we tend to feel selfish for putting ourselves before everyone else. But caring for yourself is not selfish, especially when your motive is to care for yourself so that you are then able to care for your loved ones. Selfish is defined by dictionary.com as "devoted to or caring only for oneself; concerned primarily with one's own interests, benefits, welfare, etc., regardless of others.".
Another factor in flares is not taking good care of yourself, or taking care of everyone around you at the expense of not giving yourself enough care. As women, we are taught to be the caretakers. But, one thing we, especially those of use with chronic illnesses, absolutely MUST remember is that we cannot take care of those around us if we do not meet our own needs properly as well. Sometimes, even though it may feel somewhat selfish (and against all that we are taught is part of being a great wife, mother, employee, friend, etc.), we MUST make time to care for ourselves. At times, we need to do this before we can meet the needs of those around us. It is hard to do this as we tend to feel selfish for putting ourselves before everyone else. But caring for yourself is not selfish, especially when your motive is to care for yourself so that you are then able to care for your loved ones. Selfish is defined by dictionary.com as "devoted to or caring only for oneself; concerned primarily with one's own interests, benefits, welfare, etc., regardless of others.". Here is one way of looking at it in a way that can help you feel less selfish and/or guilty about taking care of yourself before meeting the needs of others.. When you are flying somewhere, the flight attendants go over all of the rules, regulations and emergency procedures. One hard and fast rule is that should an emergency occur and the oxygen masks drop down, you are to put on your own mask before trying to help another person with theirs. You are to do this because should you not put your own mask on first, in helping another person, something could happen to keep you from being able to put your own mask and then there would be two people in need of help, rather than the original person. Had you put on your own mask before trying to help the other person, you would have eliminated your need for help. The extra few seconds that you would have taken to get your mask on likely would not have made a bit of difference to the person you were helping.
That example can be likened to you caring for your own needs before caring for the needs of those around you. By caring for yourself, you're keeping the chances that you need the help of those around you lower. Don't let your love and caring for those around you prevent you from properly caring for yourself. You are not going to be able to care for those you wish to care for from a hospital bed! And before you think that cannot or is not likely to happen to you, I thought the same thing prior to Dec. 2008.
How I Learned the Hard Way
 |
| Wayney 03/2008 The result of taking 20mg prednisone |
Cellulitis
 |
| Cellulitis left leg mid Jan 2009 |
 |
| This is my leg during the healing process in May 2009. Below the wound, I am wearing a boot to prevent heel sores |
 |
| This is not mine, but is a pic of a leg with a wound vacuum on it |
"Negative-pressure wound therapy (sometimes called "vacuum-assisted closure"). A sterile sponge is placed in the sore and covered with a sticky bandage that does not allow any air in. The small vacuum is then turned on and kept on at all times until the next treatment. The vacuum pulls drainage from the wound to help keep germs from collecting and growing there, and gently pulls the blood supply close to the surface of the sore to bring nutrients to the sore and to make new tissue grow."
 |
| My leg as of Feb 2010. As of Apr 2012 it looks the same as in this pic, minus the small sore. |
By the time the wound was considered healed, they had been having a nurse who specialized in wound care coming in and doing the care of that area. Even after it had completely healed, she cautioned that it would possibly still form small sores on it at times. It did that for at least a year afterward if not longer.
Contractures
 |
| This is how my hand looked due to the contracture, before beginning OT in Apr 2011. |

I also developed a number of joint contractures from not moving for months. My ankles are in a position of when I am lying in bed, my toes point down toward the bed. During my PT at the nursing home, Jim, my therapist, worked hard to stretch the muscles and tendons in my legs and feet in order to allow me to be able to stand and walk. I still have quite a bit of contracture in my ankles but I have more movement than I did in the beginning of my PT. Even my toes contracted and now when I walk, I basically am standing with my weight on the tips of the toes of my right foot. My left foot is not nearly as bad. Which is kinda funny as in my feet, the right side is worse. But in my hands, the left was worse than the right one. My hands contracted so that I had loose fists and could not open my hands. Then my wrists also contracted and drew my hands down so that the fist basically faced the underside of my forearm. My elbows contracted as well and were bent so that each hand rested right along my collar bone.
Feeding Tubes
 |
| This is a picture of a woman with a nasogastric feeding tube. |
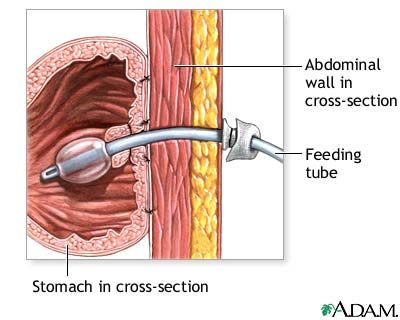 |
| Illustration of a J tube |
"a tube surgically inserted through the abdomen and into the jejunum (the second part of the small intestine). The procedure is called a jejunostomy."
 |
| My PEG tube taken Apr. 2010 |
"a tube inserted through a small incision in the abdomen into the stomach and is used for long-term enteral nutrition. One type is the percutaneous endoscopic gastrostomy (PEG) tube which is placed endoscopically. The position of the endoscope can be visualized on the outside of the patient's abdomen because it contains a powerful light source. A needle is inserted through the abdomen, visualized within the stomach by the endoscope, and a suture passed through the needle is grasped by the endoscope and pulled up through the esophagus. The suture is then tied to the end of the PEG tube that will be external, and pulled back down through the esophagus, stomach, and out through the abdominal wall. The insertion takes about 20 minutes. The tube is kept within the stomach either by a balloon on its tip (which can be deflated) or by a retention dome which is wider than the tract of the tube."
 |
| After tube removed May 2010 |
PICC Line
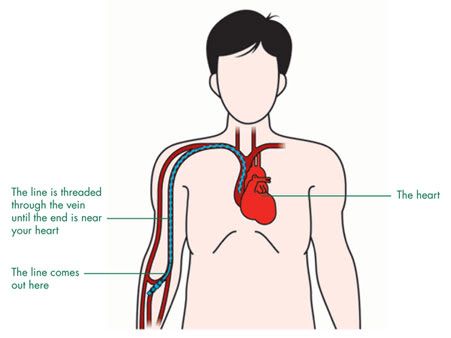 |
| Illustration of a PICC line |
 |
| Wayney in hospital Summer 2009 |
 |
| Wayney in nursing home Jan 2010 |
Life with a chronic illness (or multiple chronic illnesses) can be filled with a number of lessons. Some are learned fairly easily, some are learned by seeing the experiences of other people. Other lessons are learned the hard way. Learning these lessons the hard way means that they will more than likely stay with you. You tend not to forget the hard stuff. I know that the lessons I've had to learn the hard way: not pushing myself too hard; making sure I properly take care of myself; practicing that good self-care by decreasing stress and sleeping properly have been the lessons that have been hard for me to learn. I think the one that sticks with me the most is pacing myself during a flare. It is one of the harder ones for me to do, but I have found that if I pace myself, I don't have quite as many problems during a mild flare. Not much helps during a major flare where my RA, fibro and Sjogren's are all flaring. That is a time when I just have to ride it out and do as best I can.
 |
| Wayney at home Jan 2011 |




No comments:
Post a Comment