Health Mascot
The prompt for today was to give my health focus a mascot. I decided to make them a fictional team of superheros. Face it, dealing with these conditions takes a superhero. I am a firm believer that anyone who manages their condition(s) has to be amazing. Living with any chronic illness is tough on the person who has the illness as well as all of their loved ones. It takes a certain strength to live day in and day out
with all of what goes with these health conditions. Until one has lived with a chronic illness, they cannot imagine what its like. Even the most understanding, willing to help of loved ones can only guess what it is like for the person with the chronic illness. They get a very good picture and can most likely make a guess that is quite close to the truth, but they can't know how it feels unless they too have a chronic illness. As much as my family is awesome at understanding, accepting and helping me, they can't know what it feels like inside, especially if I cannot describe it. So using Superheroes as mascots is not a stretch! So, here are the superheroes I've found to represent the health conditions I focus on. One note: the "special weapons" sections of information are NOT my own writing! I have used medication information from articles copied from the sources I linked to under each section. I normally do not do that. but it is information about medications so it's not as if I could really supply it in my own words, as I am not a pharmacist, doctor, etc. It is used for educational purposes only.

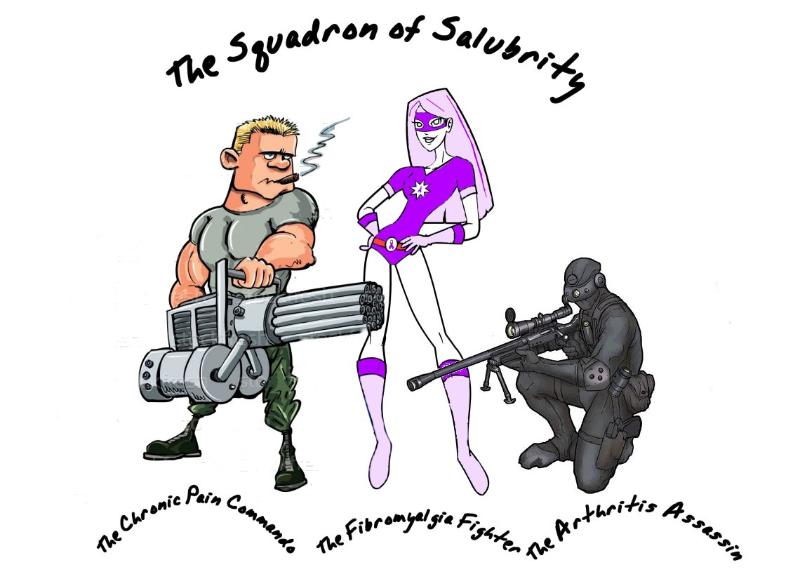 Title: Arthritis Assassin
Team: Squadron of Salubrity
Report to: Head Honcho of Health
Duties: Assist Head Honcho of Health in fighting the effects of arthritis in ALL of its forms.
Specialized Weapons:
Title: Arthritis Assassin
Team: Squadron of Salubrity
Report to: Head Honcho of Health
Duties: Assist Head Honcho of Health in fighting the effects of arthritis in ALL of its forms.
Specialized Weapons: Biological Response Modifiers (BRMs)
, Disease Modifying Anti-Rheumatic Drugs (DMARDs)
, Glucocorticoids (Cortisone-Related Drugs)
, Gout Medications
, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
, Osteoporosis Medications
Substances
that modify the body's response to infection and disease. The body
naturally produces small amounts of these substances. Scientists can
produce some of them in the laboratory in large amounts for use in
treating cancer, rheumatoid arthritis, and other diseases.
BRMs
used in biological therapy include monoclonal antibodies, interferon,
interleukin-2 (IL-2), and several types of colony- stimulating factors
(CSF, GM-CSF, G-CSF). Interleukin-2 and interferon are BRMs being tested
for the treatment of advanced malignant melanoma. Interferon is a BRM
now in use to treat hepatitis C.
The
side effects of BRM therapy often include flu-like symptoms such as
chills, fever, muscle aches, weakness, loss of appetite, nausea,
vomiting, and diarrhea. Some patients develop a rash, and some bleed or
bruise easily. Interleukin therapy can cause swelling. Depending on the
severity of these problems, patients may need to stay in the hospital
during treatment. These side effects are usually short-term and go
gradually away after treatment stops.
Brand Name
|
Generic Name
|
|
|
tocilizumab injection
|
|
|
certolizumab pegol
|
|
|
etanercept
|
|
|
adalimumab
|
|
|
anakinra
|
|
|
abatacept
|
|
|
infliximab
|
|
|
rituximab
|
|
|
golimumab
|
While
"first-line" medications (NSAIDs and corticosteroids) can relieve joint
inflammation and pain, they do not necessarily prevent joint
destruction or deformity. For patients with an aggressively destructive
form of rheumatoid arthritis, medications other than NSAIDs and
corticosteroids are needed. These "second-line" or "slow-acting"
medicines (listed below) may take weeks to months to become effective.
They are used for long periods of time, even years, at varying doses. If
effective, they can promote remission, thereby retarding the
progression of joint destruction and deformity. Sometimes a number of
second-line medications are used together as combination therapy.
Hydroxychloroquine
(PLAQUENIL) is related to quinine, and is used in the treatment of
malaria. It is used over long periods for the treatment of rheumatoid
arthritis. Side effects include upset stomach, skin rashes, muscle
weakness, and vision changes. Even though vision changes are rare,
patients taking PLAQUENIL should be monitored by an eye doctor
(ophthalmologist).
Sulfasalazine
(AZULFADINE) is an oral medication traditionally used in the treatment
of mild to moderately severe inflammatory bowel diseases, such as
ulcerative colitis and Crohn's colitis. AZULFADINE is used to treat
rheumatoid arthritis in combination with antiinflammatory medications.
AZULFADINE is generally well tolerated. Common side effects include rash
and upset stomach. Because AZULFADINE is made up of sulfa and
salicylate compounds, it should be avoided by patients with known sulfa
allergies.
Gold
salts have been used to treat rheumatoid arthritis throughout most of
this century. Gold thioglucose (SOLGANAL) and gold thiomalate
(MYOCHRYSINE) are given by injection, initially on a weekly basis for
months to years. Oral gold, auranofin (RIDAURA) was introduced in the
1980's. Side effects of gold (oral and injectable) include skin rash,
mouth sores, kidney damage with leakage of protein in the urine, and
bone marrow damage with anemia and low white cell count. Patients
receiving gold treatment are regularly monitored with blood and urine
tests. Oral gold can cause diarrhea.
Brand Name
|
Generic Name
|
|
|
leflunomide
|
|
|
sulfasalazine
|
|
|
penicillamine
|
|
|
etanercept
|
|
|
adalimumab
|
|
|
azathioprine
|
|
|
hydroxychloroquine
|
|
|
infliximab
|
|
|
methotrexate
|
|
|
auranofin
|
|
|
aurothiglucose
|
Glucocorticoids
are medications that include cortisone and related drugs. A
glucocorticoid is hormone that predominantly affects the metabolism of
carbohydrates and, to a lesser extent, fats and proteins (and has other
effects). Glucocorticoids are made in the outside portion (the cortex)
of the adrenal gland and chemically classed as steroids. Cortisol is the
major natural glucocorticoid. The term glucocorticoid also applies to
equivalent hormones synthesized in the laboratory. Glucocorticoid drugs
are also called corticosteroids.
Corticosteroids
have potent anti-inflammatory properties, and are used in a wide
variety of inflammatory conditions such as arthritis, colitis, asthma,
bronchitis, certain skin rashes, and allergic or inflammatory conditions
of the nose and eyes. There are numerous preparations of
corticosteroids including oral tablets, capsules, liquids, topical
creams and gels, inhalers and eye drops, and injectable and intravenous
solutions.
Dosage
requirements of corticosteroids vary among individuals and the diseases
being treated. In general, the lowest possible effective dose is used.
Corticosteroids given in multiple doses throughout the day are more
effective, but also more toxic, than if the same total dose is given
once daily, or every other day.
Brand Name
|
Generic Name
|
|
|
Corticosteroid Injection
of Soft Tissues & Joints
|
|
|
dexamethasone, oral
|
|
|
prednisone, oral
|
|
|
prednisolone
|
|
|
hydrocortisone, oral
|
|
|
methylprednisolone
|
There
are three aspects to the medication treatment of gout. First, pain
relievers such as TYLENOL or other more potent analgesics are used to
manage pain. Secondly, anti-inflammatory agents such as nonsteroidal
anti-inflammatory drugs (NSAIDS), colchicine, and corticosteroids are
used to decrease joint inflammation. Finally, medications are considered
for managing the underlying metabolic derangement that causes high
blood levels of uric acid (hyperuricemia) and leads to gout attacks and
kidney stones.
Brand Name
|
Generic Name
|
see below
|
NSAIDS
|
|
|
sulfinpyrazone
|
|
|
probenecid
|
|
|
colchicine
|
|
|
allopurinol
|
Nonsteroidal
anti-inflammatory drugs. These are medications that reduce inflammation
and do not contain cortisone-related compounds.
Nonsteroidal
anti-inflammatory drugs (NSAIDs) are commonly prescribed medications
for the inflammation of arthritis and other body tissues, such as in
tendinitis and bursitis. Examples of NSAIDs include ASPIRIN,
indomethacin (INDOCIN), ibuprofen (MOTRIN), naproxen (NAPROSYN),
piroxicam (FELDENE), and nabumetone (RELAFEN). The major side effects of
NSAIDs are related to the gastrointestinal system. Some 10%-50% of
patients are unable to tolerate NSAID treatment because of side effects,
including abdominal pain, diarrhea, bloating, heartburn, and upset
stomach. Approximately 15% of patients on long-term NSAID treatment
develop ulceration of the stomach and duodenum. Even though many of
these patients with ulcers do not have symptoms and are unaware of their
ulcers, they are at risk of developing serious ulcer complications such
as bleeding or perforation of the stomach.
NSAIDs are taken regularly by approximately 33 million Americans!
Brand Name
|
Generic Name
|
|
|
ibuprofen
|
|
|
flurbiprofen
|
|
|
aspirin
|
|
|
celecoxib
|
|
|
sulindac
|
|
|
oxaprozin
|
|
|
salsalate
|
|
|
piroxicam
|
|
|
indomethacin
|
|
|
etodolac
|
|
|
meclofenamate
|
|
|
meloxicam
|
|
|
fenoprofen
|
|
|
naproxen
|
|
|
ketoprofen
|
|
|
tolmetin
|
|
|
choline magnesium salicyclate
|
|
|
diclofenac
|
The
best treatment for osteoporosis is prevention. Quitting smoking and
curtailing alcohol intake are helpful. Exercise against gravity can
reduce bone loss and can even stimulate new bone formation.
Additionally, exercise increases agility, strength, and endurance;
factors that can reduce accidents. Exercise programs are individualized
and should be regular; at least several times weekly. For patients with
underlying musculoskeletal disorders, combining exercise with joint
protection techniques is important.
Calcium
supplements are useful, especially in women. Average women in the
United States receive less than 500 milligrams of calcium per day in
their diet. The recommended daily allowance (RDA) of calcium intake is
800mg per day. The National Institute of Health Consensus Conference on
Osteoporosis has recommended a calcium intake for postmenopausal women
of 1000mg per day if they are also taking estrogen and 1500mg per day if
they are not taking estrogen.
Estrogen
replacement in postmenopausal women is important in the prevention of
accelerated bone loss. Estrogen can even reverse the bone loss that
occurs after menopause. Estrogen is available orally (PREMARIN, ESTRACE,
ESTRATEST, and others) or as a skin patch (ESTRADERM, VIVELLE, and
others). Women with certain conditions, such as a history of breast
cancer, phlebitis,
or stroke may not be candidates for estrogen because of the potential
for worsening or inducing recurrences of these conditions.
Vitamin
D supplementation has been shown to be of benefit in elderly patients,
particularly those in nursing homes. This is probably due to the fact
that many patients in nursing homes are vitamin D deficient.
References:
Arthritis Medications Information on drug classes and medication lists for each class except for BRMs approve after article was written.
Common Drugs and Medications to Treat Rheumatoid Arthritis Information on BRMs not found in article above.
Title: Fibro Fighter
Report to: Head Honcho of Health
Duties: Assist Head Honcho of Health in fighting the effects of arthritis, fibromyalgia, and chronic pain.
Specialized Weapons: Non-Steroidal
Anti-Inflammatory Drugs (NSAIDs), Antidepressants, Tricyclic
Antidepressants, Selective Serotonin Reuptake Inhibitors (SSRIs), Mixed
Reuptake Inhibitors, Benzodiazepines, Other Medications For
Fibromyalgia, Symptom-Specific Drugs

NSAIDs
NSAIDs (nonsteroidal anti-inflammatory drugs) are used to treat inflammation.
Although inflammation is not a symptom of fibromyalgia, NSAIDs also relieve pain. NSAIDs include:
NSAIDs work by inhibiting prostaglandins, which play a role in pain and inflammation. These drugs, some of which are available over-the-counter,
may help ease the muscle aches of fibromyalgia. They may also relieve
menstrual cramps and the headaches often associated with fibromyalgia.
Antidepressants
Perhaps
the most useful medications for fibromyalgia are several in the
antidepressant class. Antidepressants elevate the levels of certain
chemicals in the brain, including serotonin and norepinephrine. Low
levels of these chemicals are associated not only with depression, but
also with pain and fatigue. Increasing the levels of these chemicals can
reduce pain in people who have fibromyalgia. Doctors prescribe several
types of antidepressants for people with fibromyalgia.
Tricyclic Antidepressants
When
taken at bedtime in dosages lower than those used to treat depression,
tricyclic antidepressants can help promote restorative sleep in people
with fibromyalgia. They also can relax painful muscles and heighten the
effects of the body's natural pain-killing substances called endorphins.
Tricyclic
antidepressants have been around for almost half a century. Some
examples of tricyclic medications used to treat fibromyalgia include:
Selective Serotonin Reuptake Inhibitors (SSRIs)
If
a tricyclic antidepressant fails to bring relief, doctors sometimes
prescribe a newer type of antidepressant called a SSRI. As with
tricyclics, doctors usually prescribe these for people with fibromyalgia
in lower dosages than are used to treat depression. By promoting the
release of serotonin, these drugs may reduce fatigue and some other
symptoms associated with fibromyalgia. The group of SSRIs includes:
SSRIs
may be prescribed along with a tricyclic antidepressant. Doctors rarely
prescribe SSRIs alone. Because they make people feel more energetic,
they also interfere with sleep, which often is already a problem for
people with fibromyalgia.
Cymbalta (duloxetine) is a selective serotonin and norepinephrine reuptake inhibitor (SSNRI) that is also showing promise.
Mixed Reuptake Inhibitors
Some
newer antidepressants raise levels of both serotonin and
norepinephrine, and are therefore called mixed reuptake inhibitors.
Examples of these drugs include:
Researchers are actively studying the efficacy of these drugs in treating fibromyalgia.
Benzodiazepines
Benzodiazepines
help some people with fibromyalgia by relaxing tense, painful muscles
and stabilizing the erratic brain waves that can interfere with deep
sleep. Benzodiazepines also can relieve the symptoms of restless legs
syndrome, which is common among people with fibromyalgia. Restless legs syndrome
is characterized by unpleasant sensations in the legs as well as
twitching, particularly at night. Because of the potential for
addiction, doctors usually prescribe benzodiazepines only for people who
have not responded to other therapies. Benzodiazepines include:
Other Medications For Fibromyalgia
Doctors
may prescribe other medications, depending on a person's specific
symptoms or fibromyalgia-related conditions. For example:
-
Gabapentin is being studied as a treatment for fibromyalgia.
Pregabalin (Lyrica) is the first medicine that is FDA-approved to treat fibromyalgia.
-
-
Symptom-Specific Drugs
Other symptom-specific drugs include:
Resource:
Fibromyalgia Medications - How Is Fibromyalgia Treated?
Title: Chronic Pain Commando
Report to: Head Honcho of Health
Duties: Assist Head Honcho of Health in fighting the effects of arthritis, fibromyalgia, and chronic pain.
Specialized Weapons: Medications: Mild pain, Mild to moderate pain, Moderate to severe pain, Opioids, Non-steroidal anti-inflammatory drugs, Antidepressants and antiepileptic drugs, Other analgesics; Procedures; Physical approach: Physiatry, TENS, Acupuncture, LLLT; Psychological approach: Hypnosis

Medications:
Mild Pain
Mild to moderate pain
Paracetamol/Tylenol, an NSAID and/or paracetamol/Tylenol in a combination product with a weak opioid such as hydrocodone, may provide greater relief than their separate use.
Moderate to severe pain
When
treating moderate to severe pain, the type of the pain, acute or
chronic, needs to be considered. The type of pain can result in
different medications being prescribed. Certain medications may work
better for acute pain, others for chronic pain, and some may work
equally well on both. Acute pain medication is for rapid onset of pain
such as from an inflicted trauma or to treat post-operative pain. Chronic pain medication is for alleviating long-lasting, ongoing pain.
Morphine is the gold standard to which all narcotics are compared. Fentanyl has the benefit of less histamine release and thus fewer side effects. It can also be administered via transdermal patch which is convenient for chronic pain management. Oxycodone is used across the Americas and Europe for relief of serious chronic pain; its main slow-release formula is known as OxyContin, and short-acting tablets, capsules, syrups and ampules are available making it suitable for acute intractable pain or breakthrough pain. Diamorphine, methadone and buprenorphine are used less frequently. Pethidine,
known in North America as meperidine, is not recommended for pain
management due to its low potency, short duration of action, and
toxicity associated with repeated use. Pentazocine, dextromoramide and dipipanone
are also not recommended in new patients except for acute pain where
other analgesics are not tolerated or are inappropriate, for
pharmacological and misuse-related reasons. Amitriptyline is prescribed for chronic muscular pain in the arms, legs, neck and lower back. While opiates are often used in the management of chronic pain, high doses are associated with an increased risk of opioid overdose.
Opioids
Opioid
medications can provide a short, intermediate or long acting analgesia
depending upon the specific properties of the medication and whether it
is formulated as an extended release drug. Opioid medications may be
administered orally, by injection, via nasal mucosa or oral mucosa,
rectally, transdermally, intravenously, epidurally and intrathecally. In
chronic pain conditions that are opioid responsive a combination of a
long-acting or extended release medication is often prescribed in conjunction with a shorter-acting medication for breakthrough pain, or exacerbations.
Most opioid treatment is oral (tablet, capsule or liquid), but suppositories and skin patches can be prescribed. An opioid injection is rarely needed for patients with chronic pain.
Although
opioids are strong analgesics, they do not provide complete analgesia
regardless of whether the pain is acute or chronic in origin. Opioids
are efficacious analgesics in chronic malignant pain and modestly
effective in nonmalignant pain management. However, there are associated
adverse effects, especially during the commencement or change in dose.
When opioids are used for prolonged periods drug tolerance, chemical dependency, diversion and addiction may occur.
Clinical
guidelines for prescribing opioids for chronic pain have been issued by
the American Pain Society and the American Academy of Pain Medicine.
Included in these guidelines is the importance of assessing the patient
for the risk of substance abuse, misuse, or addiction; a personal or
family history of substance abuse is the strongest predictor of aberrant
drug-taking behavior. Physicians who prescribe opioids should integrate
this treatment with any psychotherapeutic intervention the patient may
be receiving. The guidelines also recommend monitoring not only the pain
but also the level of functioning and the achievement of therapeutic
goals. The prescribing physician should be suspicious of abuse when a
patient reports a reduction in pain but has no accompanying improvement
in function or progress in achieving identified goals.
Non-steroidal anti-inflammatory drugs
The other major group of analgesics are non-steroidal anti-inflammatory drugs (NSAID). Acetaminophen/paracetamol
is not always included in this class of medications. However,
acetaminophen may be administered as a single medication or in
combination with other analgesics (both NSAIDs and opioids). The
alternatively prescribed NSAIDs such as ketoprofen and piroxicam, have limited benefit in chronic pain disorders and with long-term use is associated with significant adverse effects. The use of selective NSAIDs designated as selective COX-2 inhibitors have significant cardiovascular and cerebrovascular risks which have limited their utilization
Antidepressants and antiepileptic drugs
Some antidepressant and antiepileptic
drugs are used in chronic pain management and act primarily within the
pain pathways of the central nervous system, though peripheral
mechanisms have been attributed as well. These mechanisms vary and in
general are more effective in neuropathic pain disorders as well as complex regional pain syndrome. Drugs such as gabapentin
have been widely prescribed for the off-label use of pain control. The
list of side effects for these classes of drugs are typically much
longer than opiate or NSAID treatments for chronic pain, and many anti-epileptics cannot be suddenly stopped without the risk of seizure.
Other analgesics
Other
drugs are often used to help analgesics combat various types of pain
and parts of the overall pain experience. In addition to gabapentin, the vast majority of which is used off-label for this purpose, orphenadrine, cyclobenzaprine, trazodone
and other drugs with anticholinergic properties are useful in
conjunction with opioids for neuropathic pain. Orphenadrine and
cyclobenzaprine are also muscle relaxants and are therefore particularly useful in painful musculoskeletal conditions. Clonidine has found use as an analgesic for this same purpose and all of the mentioned drugs potentiate the effects of opioids overall.
Procedures
An intrathecal pump
used to deliver very small quantities of medications directly to the
spinal fluid. This is similar to epidural infusions used in labour
and postoperatively. The major differences are that it is much more
common for the drug to be delivered into the spinal fluid (intrathecal)
rather than epidurally, and the pump can be fully implanted under the
skin. This approach allows a higher dose of the drug to be delivered
directly to the site of action, with fewer systemic side effects.
A spinal cord stimulator
is an implantable medical device that creates electric impulses and
applies them near the dorsal surface of the spinal cord provides a paresthesia ("tingling") sensation that alters the perception of pain by the patient.
Physical approach
Physiatry
Physical medicine and rehabilitation (physiatry/physiotherapy) employs diverse physical techniques such as thermal agents and electrotherapy,
as well as therapeutic exercise and behavioral therapy, alone or in
tandem with interventional techniques and conventional pharmacotherapy
to treat pain, usually as part of an interdisciplinary or
multidisciplinary program.
TENS
Acupuncture
Acupuncture
involves the insertion and manipulation of needles into specific points
on the body to relieve pain or for therapeutic purposes. An analysis of
the 13 highest quality studies of pain treatment with acupuncture,
published in January 2009 in the British Medical Journal, concluded there was little difference in the effect on pain of real, sham and no acupuncture.
LLLT
A 2007 review published in the journal Annals of Internal Medicine
concluded low-level laser therapy has "not been shown to be effective
for either chronic or sub-acute or acute low back pain; and a 2008 Cochrane collaboration review concluded that there was insufficient evidence to support the use of LLLT in the management of low back pain.
Psychological approach
Evidence for the usefulness of behavioral therapy (BT) and cognitive behavioral therapy
(CBT) in the management of adult chronic pain is generally weak, due
partly to the proliferation of techniques of doubtful quality, and the
poor quality of reporting in clinical trials. The crucial content of
individual interventions has not been isolated and the important
contextual elements, such as therapist training and development of
treatment manuals, have not been determined. The widely varying nature
of the resulting data makes useful systematic review and meta-analysis within the field very difficult.
In 2009 a systematic review of randomized controlled trials
(RCTs) of psychological therapies for the management of adult chronic
pain (excluding headache) found that "CBT and BT have weak effects in
improving pain. CBT and BT have minimal effects on disability associated
with chronic pain. CBT and BT are effective in altering mood outcomes,
and there is some evidence that these changes are maintained at six
months;" and a review of RCTs of psychological therapies for the
management of chronic and recurrent pain in children and adolescents, by
the same authors, found "Psychological treatments are effective in pain
control for children with headache and benefits appear to be
maintained. Psychological treatments may also improve pain control for
children with musculoskeletal and recurrent abdominal pain. There is
little evidence available to estimate effects on disability or mood."
Hypnosis
A 2007 review of 13 studies found evidence for the efficacy of hypnosis
in the reduction of pain in some conditions, though the number of
patients enrolled in the studies was small, bringing up issues of power
to detect group differences, and most lacked credible controls for
placebo and/or expectation. The authors concluded that "although the
findings provide support for the general applicability of hypnosis in
the treatment of chronic pain, considerably more research will be needed
to fully determine the effects of hypnosis for different chronic-pain
conditions." (p. 283).
Resource:














